The Biology of Miscarriage
Most pregnancy losses are unavoidable and not the result of an embryo being 'mis-carried'. Here's a compassionate, biological reframing.
This week’s post is a personal one and may resonate with some readers. My hope is that exploring the biology of miscarriage will bring both comfort and understanding to those who need it.
Before diving in, I want to highlight a post from Evolution and Psychiatry featuring Anne-Laure Le Cunff’s insightful work on ADHD. It offers a strengths-based perspective, reframing ADHD as an evolutionarily adaptive trait. This approach invites us to move beyond a deficit-focused lens and embrace the unique abilities that individuals with ADHD bring to our modern world.
Why the word 'miscarriage' is misleading
This is a topic close to my heart. Like so many other women, I've experienced pregnancy loss — for me, it came during an IVF journey that had already felt long and challenging. As I journeyed through the weeks that followed, women all around me shared their own stories of loss. I was struck by just how common the experience is, but also by the prevalence of guilt and self-doubt. To echo the words of Taylor Swift: "Did some force take you because I didn't pray?" Or was it because I was stressed last week, ate that salmon, didn’t exercise enough, or perhaps exercised too much?
Self-blame is a common response, but a closer look at the science absolves us of personal responsibility and is, ultimately, freeing. Most pregnancy losses aren’t caused by anything the person carrying the pregnancy did or didn’t do. Instead, they’re overwhelmingly the result of chromosomal abnormalities — issues that prevented the embryo from developing because it didn’t have the correct ‘instruction manual’ needed to grow into a healthy baby.
This reframing matters. Even the term ‘miscarriage’ implies fault, as though the womb-holder ‘mis-carried’ the pregnancy. But when we look at the biology, it becomes clear that this term is misleading. Let’s explore why, and understand how the science of pregnancy loss can lead to a kinder and more accurate narrative.
Causes of pregnancy loss
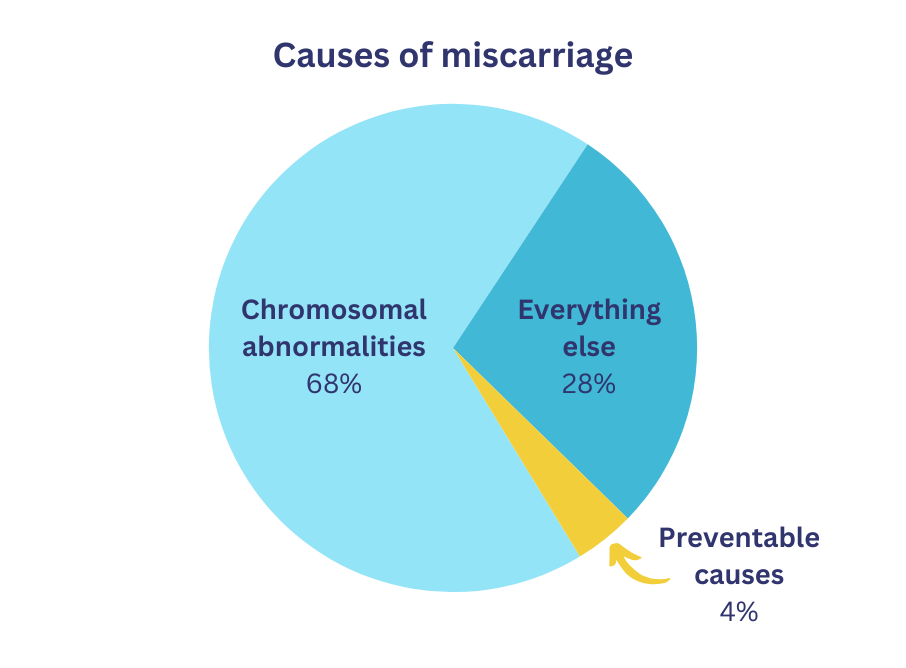
Recent studies show that up to 68% of pregnancy losses are caused by chromosomal abnormalities.1 These are random errors in the embryo's DNA that occur during conception or early cell division, and are entirely unpreventable. The remaining 32% of pregnancy losses result from a diverse range of factors. While the vast majority of these other factors are also unpreventable, our focus today is on chromosomal abnormalities, as these are by far the most common cause of pregnancy loss.
Chromosomal abnormalities
Pregnancy begins with the combination of genetic material from the sperm and egg to form an embryo. Each contributes 23 chromosomes, creating a full set of 46. These chromosomes act as the embryo’s instruction manual, containing all the information needed for development. When the genetic material combines correctly, the embryo is considered 'euploid' — it has the right number and structure of chromosomes. Euploidy is essential for the embryo to grow and thrive.

Errors can occur before or during fertilisation or during early cell division, which lead to an embryo that has too many or too few chromosomes, or structural defects within the chromosomes. This is called ‘aneuploidy’. In most cases, these abnormalities happen randomly and are not influenced by the actions of the person carrying the pregnancy. The same biological processes that create our unique individuality, through the random assortment of chromosomes from Mum and Dad, also lead to aneuploidy in some embryos.
How chromosomal abnormalities cause pregnancy loss
An embryo containing the correct number and structure of chromosomes has a complete instruction manual for the complex process of cell division, organ formation, and overall growth. However when an embryo is aneuploid — having too many or too few chromosomes — these instructions are incomplete or contradictory. This prevents the embryo from progressing through critical developmental milestones.
Unlike some biological processes that can be corrected by the body, an aneuploid embryo cannot develop into a healthy baby, even in the most supportive environment. Even in a 'perfect womb', if there were such a thing, these embryos would not be viable.
The stage at which an aneuploid pregnancy will end depends on which section of the embryo's DNA is abnormal. If a critical section is missing, the pregnancy might end very early (or the embryo might not even implant). However, if the chromosomal abnormality affects a gene that's not needed until later in embryonic development, the pregnancy might continue for the first few months.
How common are chromosomal abnormalities?
Research shows that approximately 47-52% of all human embryos are aneuploid (chromosomally abnormal), though most of these don't make it to implantation.2 Individual rates of aneuploidy vary with maternal age – but even young parents still have aneuploidy rates of about 30%. This high rate of chromosomal abnormalities reflects the inherent variability and randomness of reproduction, which is necessary to create the incredible genetic diversity we see around us. But the same variability and randomness that have given birth to the remarkable diversity of life on Earth also occasionally lead to outcomes incompatible with life. Such is the beauty and fragility of genetic variation.
Fortunately, most aneuploid embryos don’t make it to implantation. Studies suggest that the majority either arrest in development during early cell division stages (prior to implantation) or fail to establish the biochemical communication required for implantation.3
A compassionate reframing
When we understand that most pregnancy losses are due to factors beyond anyone’s control, it becomes clear that in most cases the womb-holder did not ‘mis-carry’ anything. They gave their body to provide the best environment possible for the pregnancy to thrive. If the embryo couldn’t survive, it’s most likely because genetic variation processes resulted in an incomplete set of instructions, or one of several other equally unavoidable causes.
‘Miscarriage’ is a medical term, defined as the spontaneous loss of a foetus before the 20th week of pregnancy. While it remains important to have universal medical definitions, it can be helpful to shift our language when appropriate. By referring to miscarriage in terms like ‘pregnancy loss’ or ‘embryo loss’ we provide a more compassionate framing, remove the implied blame, and create space for understanding and healing. This also opens the door to greater awareness of the biological complexity behind pregnancy loss. This reframing matters.
Healing after pregnancy loss
For those who have experienced pregnancy loss, understanding the biology can be a powerful step toward healing. Here are three key points to remember:
Most pregnancy losses are unpreventable. Chromosomal abnormalities are random and beyond anyone’s control, as are almost all other causes of pregnancy loss.
Pregnancy loss is common. About 15% of known pregnancies end in loss,4 making it a shared experience for many. You’re not alone.
It’s okay to grieve. Whether the loss occurred at seven weeks or seventeen, it’s a significant loss and grief is a valid response.
If you’ve experienced pregnancy loss, I see you, and I honour your story. It’s not your fault, and you’re not alone. By understanding the biology and shifting our language, we can build a culture of informed compassion.
Support resources for families experiencing pregnancy loss.
If you found this article meaningful, I invite you to share it with someone who might need these words. Together, we can foster a better understanding of pregnancy loss and support one another with compassion and care.
Essers, R. et al. Prevalence of chromosomal alterations in first-trimester spontaneous pregnancy loss. Nature Medicine 29, 3233–3242 (2023).
Wang, Y. et al. Identification of chromosomal abnormalities in early pregnancy loss using a High-Throughput Ligation-Dependent probe Amplification–Based assay. Journal of Molecular Diagnostics 23, 38–45 (2020).
Nair, J. et al. Preimplantation genetic testing for aneuploidy (PGT-A)—a single-center experience. Journal of Assisted Reproduction and Genetics 39, 729–738 (2022).
Beebeejaun, Y. et al. P-524 Ethnicity and aneuploidy rates in a global perspective: a comparative genomic study of 16,543 embryos from the United Kingdom, India and Japan. Human Reproduction 39, (2024).
McCoy, R. C. et al. Meiotic and mitotic aneuploidies drive arrest of in vitro fertilized human preimplantation embryos. Genome Medicine 15, (2023).
Regin, M. et al. Complex aneuploidy triggers autophagy and p53-mediated apoptosis and impairs the second lineage segregation in human preimplantation embryos. eLife 12, (2024).
Quenby, S. et al. Miscarriage matters: the epidemiological, physical, psychological, and economic costs of early pregnancy loss. The Lancet 397, 1658–1667 (2021).



